Hysterectomy
Hysterectomy is a surgical treatment for conditions that affect the uterus. There are many types of hysterectomies performed. Some are completed through abdominal incisions and some without. The type of hysterectomy depends on the condition, and the specific type of performed also determines the after-effects and recovery.

Hysterectomy is considered the ultimate cure for many conditions that affect the uterus but is nevertheless a major surgical procedure. Alternatives to hysterectomy are considered thoroughly before a hysterectomy is recommended. Nevertheless, hysterectomy is one of the most common surgical procedures done in this country
What is a hysterectomy?
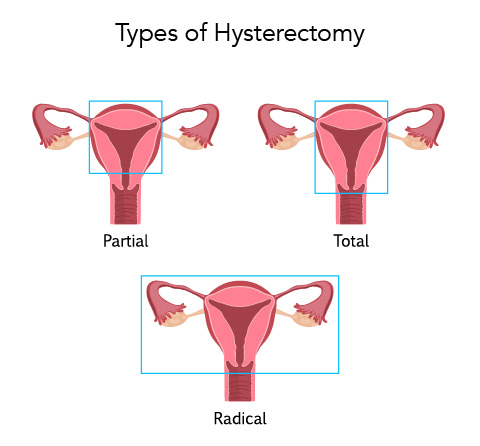
Simply, hysterectomy means removing the uterus. Partial hysterectomy means that part of the uterus is removed, the part that contains the lining and is responsible for most causes of bleeding. Total hysterectomy means removing the entire uterus. That means the lining and the cervix. Removing the uterus, whether total or partial, does not mean that the ovaries are removed. When appropriate the ovaries may be removed at the time of a hysterectomy, but not always. After any type of hysterectomy a woman is no longer able to become pregnant.
Why would I have a hysterectomy?
Hysterectomy may be done to treat many conditions that affect the uterus:
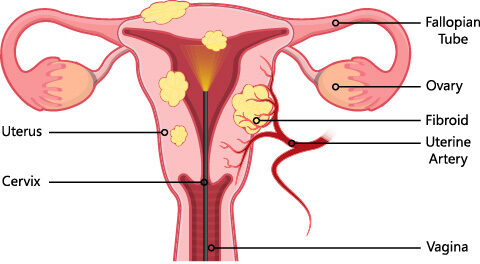
- Uterine fibroids
- Endometriosis
- Pelvic support problems (such as uterine prolapse)
- Abnormal uterine bleeding
- Cancer
- Chronic pelvic pain
Hysterectomy is major surgery, and as with any major surgery, it carries risks. For many of the problems listed previously, other treatments can be tried first.
How is a hysterectomy done?
A hysterectomy can be done in different ways. The way a hysterectomy is performed depends on the reason for the surgery and other factors, including your general health. Sometimes it is not possible to know before the surgery how the hysterectomy will be performed. Conditions which can not be assessed prior to the surgery can influence which technique would be the safest. The following video shows a robotic hysterectomy being performed by Dr. Genevieve Fairbrother.
Vaginal Hysterectomy
In a vaginal hysterectomy, the uterus is removed through the vagina. With this type of surgery, you will not have an incision on your abdomen. Because the incision is inside the vagina, the healing time may be shorter than with abdominal surgery. There may be less pain during recovery. Vaginal hysterectomy causes fewer complications than the other types of hysterectomy and is a very safe way to remove the uterus. It also is associated with a shorter hospital stay and a faster return to normal activities than abdominal hysterectomy.
A vaginal hysterectomy is not always possible. For example, women who have adhesions from previous surgery or who have a very large uterus may not be able to have this type of surgery.
Abdominal Hysterectomy
In an abdominal hysterectomy, the doctor makes an incision through the skin and tissue in the lower abdomen to reach the uterus. The incision may be vertical or horizontal.
This type of hysterectomy gives the surgeon a good view of the uterus and other organs during the operation. This procedure may be chosen if you have large tumors or if cancer may be present. Abdominal hysterectomy may require a longer healing time than vaginal or laparoscopic surgery, and it usually requires a longer hospital stay.
Laparoscopic Hysterectomy
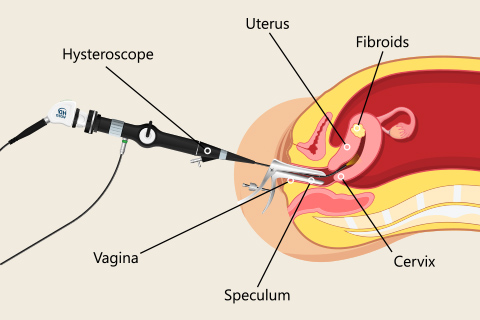
In a laparoscopic hysterectomy, a laparoscope is used to guide the surgery. A laparoscope is a thin, lighted tube with a camera that is inserted into the abdomen through a small incision in or around the navel. It allows the surgeon to see the pelvic organs on a screen. Additional small incisions are made in the abdomen for other instruments used in the surgery.

There are three kinds of laparoscopic hysterectomy:
- Total laparoscopic hysterectomy — A small incision is made in the navel for the laparoscope, and one or more small incisions are made in the abdomen for other instruments. The uterus is detached from inside the body. It then is removed in small pieces through the incisions, or the pieces are passed out of the body through the vagina. If only the uterus is removed and the cervix is left in place, it is called a supracervical laparoscopic hysterectomy.
- Laparoscopically assisted vaginal hysterectomy (LAVH) — A vaginal hysterectomy is done with laparoscopic assistance. For example, the ovaries and fallopian tubes may be detached using laparoscopy, and then the uterus is detached and all of the organs are removed through the vagina.
- Robot-assisted laparoscopic hysterectomy — Some surgeons use a robot attached to the laparoscopic instruments to help perform the surgery. It allows for more complex cases to be performed in a minimally invasive fashion allowing for faster patient recovery. Please review the section under robotic surgery.
Laparoscopic surgery has some benefits over abdominal surgery:
- The incisions are smaller, and there may be less pain.
- The hospital stay after laparoscopic surgery may be shorter.
- Quicker return to normal activities.
- The risk of infection is lower.
There also are disadvantages. It often takes longer to perform laparoscopic surgery compared with abdominal or vaginal surgery. The longer you are under general anesthesia, the greater the risks for certain complications. Also, there is an increased risk for bladder injury in this type of surgery.
Preparing for a hysterectomy
It is helpful to know what to expect before any major surgery. A physical exam is performed a few weeks before your surgery. Within 2 weeks of the surgery a Preop Appointment is scheduled with your physician to discuss and finalize plans for the type of hysterectomy to be performed and to be certain all questions are addressed.
Lab tests may be done at or after the preop appointment. A chest X-ray or electrocardiography (ECG) may need to be done for some patients.
Before any major surgery the use of all medications, including over the counter medicines, vitamins and supplements is reviewed to determine how they will affect the surgery. Some medications and supplements can cause complications during the surgery and may be discontinued on the day of surgery or earlier.
A laxative may be recommended before the day of surgery. Eat lightly the day before.
DO NOT EAT OR DRINK ANYTHING FOR 8 HOURS PRIOR TO SURGERY UNLESS SPECIFICALLY INSTRUCTED BY YOUR DOCTOR.
Some medications are given on the morning of surgery with a sip of water only.
On the day of surgery, the following things may happen:
- A needle is placed in the arm, wrist, or hand. It is attached to a tube called an intravenous (IV) line that will supply fluids, medication, or blood.
- An antibiotic to prevent infection.
- Special stockings or devices may be placed on the lower legs to prevent deep vein thrombosis (DVT). This condition is a risk with any surgery. Women at high risk of DVT may be given a drug to prevent blood clots from forming in the legs.
- Monitors will be attached before anesthesia is given. Either general anesthesia, which puts you to sleep, or regional anesthesia, which blocks out feeling in the lower part of your body will be used before the surgery begins.
- Pubic hair may be clipped. You may be awake or asleep while this is done.
- Before you are given anesthesia, you likely will be asked to state your name, the type of surgery you are having, or other information. This standard procedure, called a “time-out,” is done to ensure that the right surgery is being done on the right patient.
- A thin tube called a catheter will be placed in your bladder after you are comfortable. The catheter will drain urine from your bladder during the surgery.
What are the risks?
Hysterectomy is one of the safest surgical procedures. But as with any surgery, problems can occur:
- Infection
- Bleeding during or after surgery
- Injury to the urinary tract or nearby organs
- Blood clots in the veins or lungs
- Problems related to anesthesia
- Death
Some problems related to the surgery may not show up until a few days, weeks, or even years after surgery. These problems include bowel blockage from scarring of the intestines or formation of a blood clot in the wound. These complications are more common after an abdominal hysterectomy.
Some people are at greater risk of complications than others. For example, someone with an underlying medical condition may be at greater risk for problems related to anesthesia. An assessment of risks for complications is made prior to surgery and preventive measures are taken. These risks are discussed with the doctor at the preop appointment.
Recovery
After a hysterectomy, a person may need to stay in the hospital for a few days. The length the hospital stay will depend on the type of hysterectomy and how it was performed.
A person is urged to walk around as soon as possible after your surgery. Walking will help prevent blood clots in the legs. They may receive medicine or other care to help prevent blood clots.
A person can expect to have some pain for the first few days after the surgery. They will be given medication to relieve pain. It is common to have some bleeding and discharge from the vagina for several weeks. Sanitary pads can be used after the surgery.
During the recovery period, it is important to follow recovery instructions carefully to allow proper healing. Be sure to get lots of rest, and do not lift heavy objects until your doctor says you can. Do not put anything in your vagina during the first 6 weeks. That includes douching, having sex, and using tampons.
Your doctor will help plan your return to normal activities. Slowly increase activities such as driving, sports, and light physical work. If you can do an activity without pain and fatigue, it should be okay. If an activity causes pain, discuss it with your doctor.
Even after your recovery, you should continue to see your health care provider for routine gynecologic exams and general health care. Depending on the reason for your hysterectomy, you may still need pelvic exams and Pap tests.
Effects of Hysterectomy
Hysterectomy can have both physical and emotional effects. Some last a short time. Others may last a long time. You should be aware of these effects before having the surgery.
The ovaries are the glands that produce estrogen, a hormone that affects the body in many ways. Depending on your age, if your ovaries are removed during hysterectomy, you will have signs and symptoms caused by a lack of estrogen. A discussion of the possible need for hormone treatment is discussed at the preop appointment.
Physical Effects
After hysterectomy, the menstrual period will stop. In some cases of supracervical or partial hysterectomy menstrual bleeding can continue, but at a much lighter level than prior to the hysterectomy. If the ovaries are left in place and a woman has not yet gone through menopause, the ovaries will still produce estrogen and will continue to do so until they stop functioning naturally.
Emotional Effects
It is not uncommon to have an emotional response to hysterectomy. How you will feel after the surgery depends on a number of factors and differs for each woman.
Some women feel depressed because they can no longer have children. If depression lasts longer than a few weeks, see your health care provider. Other women may feel relieved because the symptoms they were having have now stopped.
Sexual Effects
Some women notice a change in their sexual response after a hysterectomy. Because the uterus has been removed, uterine contractions that may have been felt during orgasm will no longer occur.
Some women feel more sexual pleasure after hysterectomy. This may be because they no longer have to worry about getting pregnant. It also may be because they no longer have the discomfort or heavy bleeding caused by the problem leading to hysterectomy.
Some women wish to have a supracervical hysterectomy because they think it will have less of an impact on their sexual response compared with a total hysterectomy. Whereas sexual response is different for every woman, research comparing women who have had total hysterectomies with those who have had supracervical hysterectomies has shown that there is no difference in sexual response and orgasms in women who have had the two types of surgery.
If the ovaries are removed before menopause, you will experience effects caused by lack of estrogen. These effects are similar to those of menopause and include hot flashes, vaginal dryness, and sleep problems. However, symptoms may be more intense than what you would experience if you went through menopause over a few years, as is normal. You also may be at risk of a fracture caused by osteoporosis at an earlier age than women who go through natural menopause.
Most women who have these intense symptoms can be treated with estrogen therapy. Estrogen therapy is given in several different ways, including as a pill, injection, skin patch, vaginal cream, or vaginal ring. The form chosen depends on your specific symptoms. It is important to talk to your health care provider about all of the options and which ones are right for you.
In Summary
Hysterectomy is just one way to treat uterine problems. It is major surgery and carries some risks. For some conditions, other treatment options are available. For others, hysterectomy is the best choice. Your health care provider can help you weigh the options and make a decision.
Let's stay in touch
Our monthly newsletter keeps you up-to-date on healthy lifestyle, latest news, and our practice.